|
|
Report on efficacy of smoking
cessation medication and therapies
(click on any image for a larger view)
|
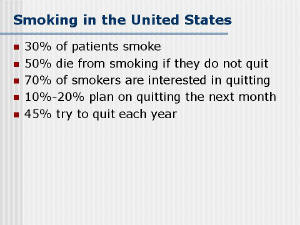 |
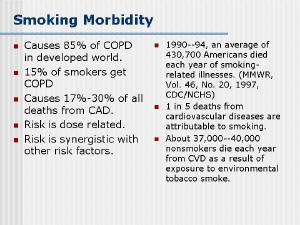
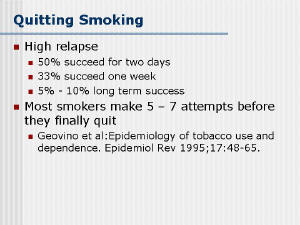
| Despite 36 years of Surgeon General warnings, 23.5%
of adults still smoke in the United States [1]. An estimated 430,700
Americans die each year from diseases caused by smoking [2]. Smoking
is responsible for an estimated one in five U.S. deaths and costs
the U.S. at least $97.2 billion each year in health care costs and
lost productivity. While cigarette companies have finally admitted
that cigarette smoking is addictive, and pharmaceutical companies
have produced and marketed several smoking cessation products, the
success rate of smoking cessation is low. Just as hypertension and
diabetes often require more then one medication for adequate
control, successful smoking cessation may require multiple therapies
for success.. |
|
 |
| Physician advice to encourage smoking cessation has
been studied extensively over the last 15 years. There have been
several large studies of physician advice that have shown quit rates
of up to 10% [9,10]. Providing patients with printed smoking
cessation information has some limited efficacy in helping smokers
to quit, but cessation rates are not high [11 Follow-up for patients
trying to quit smoking can increase the effectiveness of physician
advice and double cessation rates. |
|
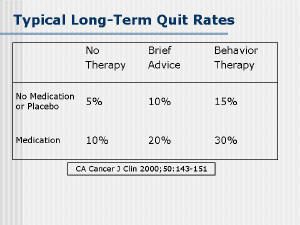 |
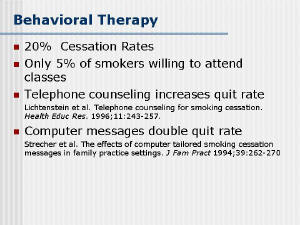
| Behavioral therapy as a means of smoking cessation
has been studied extensively, and cessation rates average 20% for
patients willing to participate in such therapy. For example, Lando
et al. [16] found that the quit rates with the American Lung
Association and American Cancer Society programs were 16% and 22%,
respectively, at one year. The main disadvantage of this approach is
that relatively few smokers (about 5%) are interested in attending
classes at any given time [17]. |
|
 |
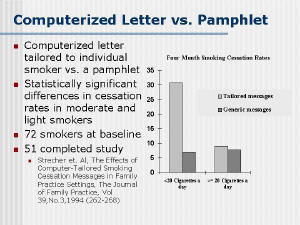
| Simple computer-tailored cessation messages may be
an effective alternative for behavioral support. Strecher et al.
[18] sent either a customized letter based on an interview from the
doctor’s office or a generic “Quit for Good” pamphlet from the
National Cancer Institute. The four-month cessation rates were 30.7%
vs. 7.1% for smokers who smoke less than 20 cigarettes a day and 9%
vs. 7.7% for those who smoke more than 20 cigarettes a day. A second
study by the same author showed that adult smokers interested in
quitting on their last exam had a 19.1% vs. 7.3% (<20 cigarettes a
day) 6-month cessation rate if they were given a tailored letter vs.
no letter. Interestingly, for smokers of more that one pack of
cigarettes per day, the quit rate was not improved (7.3% vs. 9.8).
Other studies confirm the utility of expert systems which generate
tailored cessation messages (in the form of letter or pamphlet) in
quitting [19,20,21,22]. |
|
 |
| The ease of once or twice a day dosing makes drug
therapy a very attractive method of smoking cessation; however, use
of drugs without concomitant behavioral interventions, and
unrealistic expectations on the part of patients and physicians,
tend to compromise the results of drug therapy. The most common
medication used for smoking cessation has been in the form of
nicotine replacement. Other medications include antidepressants
[26], both as single agents and in combination with nicotine
replacement. |
|
 |
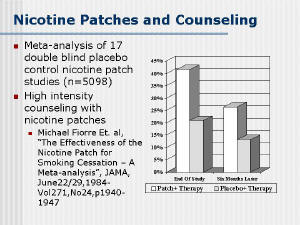
| Nicotine replacement is available as a gum, patch,
nasal spray, and inhaler. The efficacy of nicotine replacement
products is similar, with each agent leading to a doubling of the
cessation rate versus placebo. The use of the patch has been shown
to be cost-effective [30]. The product inserts for all transdermal
nicotine products indicate that they should be used as part of a
behaviorally-based cessation program. However, many patients receive
the patch without any physician advice or behavioral support [30];
without behavioral help, studies have shown very low quit rates with
nicotine patch (on the order of 5%). A meta-analysis of the
effectiveness of the nicotine patch by Fiore et al. showed that
subjects were more likely to become abstinent if counseling was a
major intended reason for patient contacts, if there were at least
weekly patient meetings in the first 4 weeks of treatment and if
there were at least seven meetings in the first 12 weeks of
treatment [31]. |
|
 |
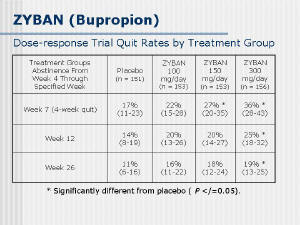
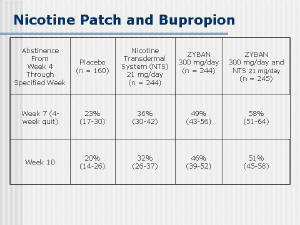
| Of the anti-depressant medications available, only
Bupropion has been approved by the FDA for smoking cessation. It
works on both the dopamine and norepinephrine transmitter systems (Zyban;
GlaxoSmithKlein; Research Triangle Park, NC). Zyban was developed
specifically for smoking cessation, and comes with a smoker support
program that includes messages on quitting and relapse prevention
[32]. Bupropion at 300 mg/day showed a 36% quit rate at 4 weeks
(n=156) but only a 19% 26 week quit rate. When combined with the
nicotine patch, a 58% 4 week quit rate was achieved. Follow-up to 1
year suggested a continued benefit to bupropion therapy [33]. |
|
 |
| However, the costs of bupropion therapy are
relatively high. Zyban, the most effective medication, costs $79.73
per month, with a standard 3-month therapy costing $239.19.
Transdermal nicotine patches cost about $3 per day, or $270 for a
12-week program. If those two therapies are combined, as suggested
by the study included in the PDR for Zyban, over $500 would be spent
to help quit smoking, with only a 58% short-term quit rate. While
this may seem high, a one pack-a-day smoker ($4/pack) will spend
$120 per month or $1,460 annually. Nevertheless, the short-term
expense is often perceived as prohibitive to the smoker |
|
 |
| As discussed above, most smoking cessation efforts
have consisted of short-term, acute interventions, and have had
limited success. However, studies show that when smoking cessation
plans incorporate long-term reinforcement of smoking cessation
goals, the quit rates can increase significantly. In a study by
Russell et al., general practitioners trained in simple smoking
cessation techniques had double the rate of decline in overall
smoking prevalence compared to brief advice-only practices [34].
Solberg et al. [35] organized a family practice to identify smokers,
systematize brief advice following a stages-of-change model, and
simplify follow-up. They found that the overall quit rate was 20%
over a 2-year period. |
|
 |
| In addition, there are indications that the ability
to quit and stay quit is associated with a number of psychosocial
and demographic variables [38,39]. For example, the majority of
studies have found that men are more likely to quit than women
[38,39,40], although data are equivocal [41,42,43]. Being married
also seems to facilitate quitting and sustained cessation [39,40],
although other forms of social support have been found to be
beneficial as well [38]. Conversely, negative support from any
source has been shown to be deleterious [44]. Not surprisingly, the
number of other current smokers in the household has been shown to
be negatively correlated with ability to quit and prevent relapse
[39]. Additionally, the presence of smoking-related environmental
cues (such as ashtrays and cigarette lighters) predicted lower
cessation success rates [37]. Overall, these results suggest that
smoking cessation programs which are responsive to the particular
needs and presses of individual smokers would have a greater chance
of success. Similarly, because more intensive treatments are
associated with better outcomes [56], a long-term behavioral
intervention that would be as easy to use as a daily pill or patch
should considerably increase rates of smoking cessation and
abstinence.
Click Here to See Rererences (requires Adobe Acrobat).
|
|
|